After caring for two parents with dementia, what I believe is that most doctors lean toward life extending measures and often don’t stop and consider the outcomes beyond the immediate resolution to an issue.
I watched as my Dad recovered from hip surgery and was cognitively a different man. He was in great physical health before the surgery (he broke his hip playing racquetball), but we all noticed a decline in his ability to hold a conversation or discuss the finances afterward. He was eventually diagnosed with Alzheimers but the years leading up to his diagnosis was filled with dozens of visits to primary care physicians, and even a neurologist, who dismissed all of our concerns about the changes in our Dad’s thinking and behavior. There really wasn’t a choice about the surgery to make since he was in good shape and had not been diagnosed cognitive issues, but the drastic change has me wondering about surgery later in life. My Dad was 76 when he had this surgery.
A recent report Major surgeries linked to small decline in mental functioning in older age confirms that a decline has been proven. However, they do believe for patients who are developing a brain disease the outcome would be more pronounced. That was definitely true with my Dad.
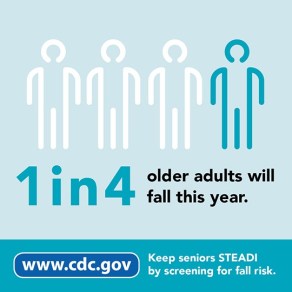
When Mom fell at 83 and the orthopedic surgeon demanded I lift Mom’s “Do Not Resuscitate” order so she could perform surgery, I balked. I had to ask for the social worker and an internist so I could convey that there is no way my Mom would be in a better place after surgery. She was living in a Memory Care community, had clearly had another stroke and had no idea who I was any longer, and mending her hip would most likely be too difficult for her to survive. As I was pushing back for them to give me options, they worked on getting my mom approved for surgery. Thankfully, the testing ultimately proved she would most likely never make it through the operation. I was able to follow the wishes she conveyed to me over decades as well as spelled out in her medical directives. Mom was moved into hospice care and died two weeks later.
What frustrated me was that there were no discussions about outcomes, just a swift recommendation to fix what was broken.
Too many families have found they end up with increased medical expenses and loved ones that are living, but don’t have the quality of life they expected after surgery in later life. Some admit that they wish they had know both the good and bad possible outcomes — but that isn’t currently how most medical consults currently work.
A few Emergency Rooms are now adding in a “Geriatric Team” to better serve those individuals coming into their hospitals and have a lot more to consider than just fixing the obvious medical emergency. The most important consideration is the what could happen and the life to be lead after. Should you be in this situation, please demand you get both the best- and worst-case options. Recommended.